Ankle Case 9 History/Physical Exam
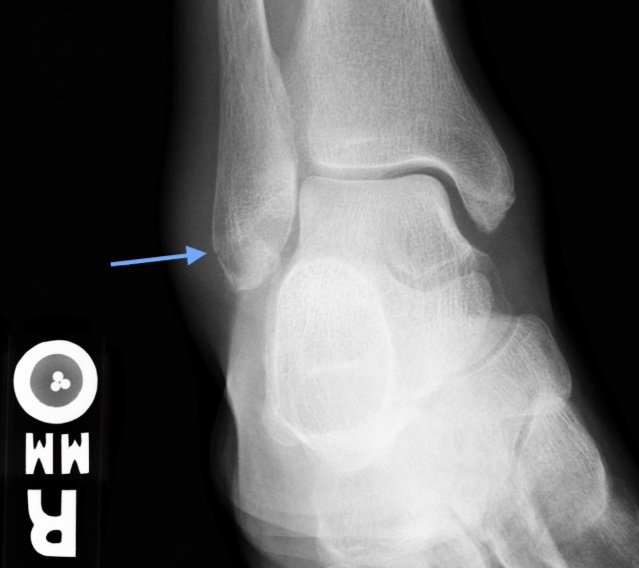
Weber A Fracture
History and Physical Exam
Patients typically have pain, swelling, bruising, and decreased mobility with distal fibular fractures. Patients may still be able to bear weight and ambulate depending on the Weber type, so this does not rule out a fracture. Weber A fractures most commonly occur from ankle inversion.
Exam will often reveal edema, ecchymosis, tenderness to palpation, and decreased range of motion of the ankle. Edema is the most common sign in ankle fractures but the degree of swelling is not reliable in predicting the presence of the fracture. There is significant overlap in clinical presentations of ankle sprains and fractures so the threshold for ordering x-rays should be very low. The Ottawa Ankle Rules can be used as evidence-based support when films seem unnecessary. Add dedicated foot x-rays for patients with metatarsal tenderness.
Make sure to assess the medial malleolus for tenderness indicative of a higher-grade sprain or potentially less stable fracture. Examine the proximal fibula in all ankle injuries to avoid missing a Maisonneuve fracture (the ankle injury is almost always more painful than the proximal fibula fracture!) and order plain films of the entire fibula for any proximal fibula tenderness.
Complete a thorough neurovascular exam, skin assessment, and visual inspection. In the event of neurovascular compromise, skin tenting, or obvious deformity.